Before my diagnosis back in 2005, I had been sick for months. I knew nothing about diabetes (oh how much has changed!). In those months, I’d told myself that even though I could barely get out of bed, was losing weight rapidly, and once passed out in the library for hours, I was probably fine. Turns out, I was not. By the time I was diagnosed with type 1 diabetes (T1D), I was in diabetic ketoacidosis, which means that my body had started to burn muscle and my blood had become overly acidic due to a buildup of ketones. As a person with T1D, I am at risk of this life-threatening condition throughout the course of my life if I experience any interruption to my insulin, including if being sick means that I cannot take insulin as usual.
I preface with this because I want you to know that seeking help is not something that comes naturally to me – at least not until things get really bad. Which is why I was surprised when, overcome with intense dizziness and nausea, I found myself on all fours in the back of a plane yelling “Help!”
It was about a year ago when my friend (who is also my colleague), and I were on a flight back from Germany where we had participated in a conference talking about the need for equity when it comes to closed-loop insulin delivery technology. If that’s confusing, I’ll explain, so stick with me. We were approaching the last leg of our journey, headed back to London to spend one night in the airport hotel before I flew back to the States, and she returned to her town.
It could have been dinner the night before, it could have been our midday snack, it could have been travel stress or any number of things – the point is, I got violently ill on the plane. I will not go into details of that except to say, when I cannot keep food down, I run a greater risk of becoming dangerously dehydrated and going into DKA. If I cannot eat/absorb food, taking insulin becomes dangerous because of the risk of low blood sugar, but if I don’t get enough insulin, my risk of DKA is greatly increased. It can be a dangerous loop. That is why, at around 11 pm, when my friend and I had finally checked into our airport hotel, she suggested we consider a trip to the ER. This brings me to what I have identified as the three key components to my personal sick day wellness strategy with T1D.
1. Having a detailed plan
When I was first diagnosed and in the few years after, I prepared extensively for travel. As I became more comfortable with diabetes management over the years, I let some of my preparation slide. While experiencing less anxiety over what could go wrong has been really great, preparing for what could go wrong is still essential for me, which I was reminded of on this trip. I was also reminded that the time to prepare is when I am well. Luckily, I had support, but if I had been traveling solo, as I have in the past, I could have ended up in really bad shape.
2. Willingness to accept help
I admit that I was resistant to the idea of going to the ER. For the first18 years of my life I did not have T1D and I dealt with sickness differently. But my friend has weathered more sick days with T1D than I, and I really trust her. Once she finally convinced me, she called an Uber and set the wheels in motion. When we climbed in, she told the driver where we needed to go, she let the front desk know that we were checking out and would not return. I simply languished beside her as she orchestrated my safe passage to the ER. It was also she who sat next to me in the ER for 6 – 8 hours and reminded me to check my ketones, check my blood sugar, and generally kept an eye on me.
3. Available help from someone understands diabetes and can be your advocate
The other thing about having help from this friend was that she really gets diabetes. She knew what to say to the staff at the ER to get them to take my concerns seriously. She knew that my rising ketone levels were a problem. She minimized nothing and was an advocate for me when I could not be. I have thought about what I might do if I was alone in this situation and identified a few things I learned from her that I will carry forward, specifically knowing where the nearest ER is anywhere I go, and having an up-to-date sick day note that specifies what I need if I am sick. Even though I might know no longer need to reference these as written guidelines, it’s helpful to have them at the ready for medical providers or others I might be traveling with. Before I go on my next trip, I will do preparatory work ahead of time, when I’m well, in order to be that stable friend for myself if I need to be. *This post’s featured image is one of us a few hours before I became ill.
4. Supportive technology or access to supplies
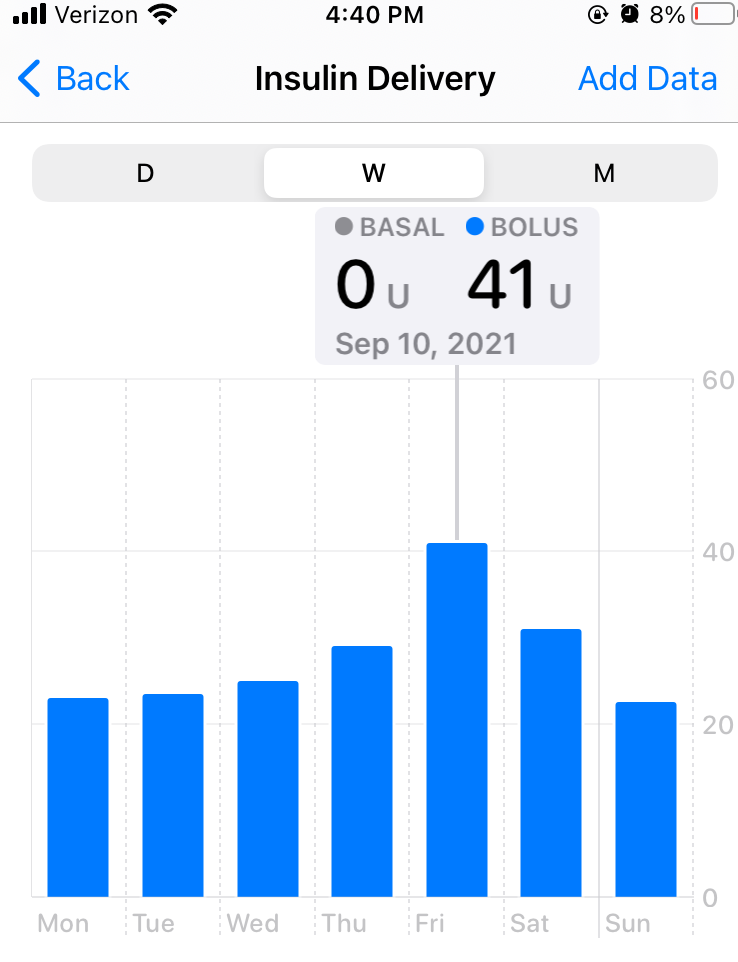
This one I want to spend a little bit more time on. For the past year, I have used the Omnipod 5 system in conjunction with the Dexcom 6 CGM. This means my insulin pump, which delivers my insulin, can communicate with my continuous glucose monitor (CGM), which measures my blood sugar. This allows my insulin pump to automatically adjust my basal insulin, which is the continuous background insulin that I need, to help me stay closer to my target blood sugar range. There are still a lot of inputs required from me such as carb counting and bolusing for what I eat, adjusting based on my physical activity, and the logistics of site changes and troubleshooting. The pods, which I change every three days, are expensive, even with insurance, costing $140 a month. However, while in grad school, the amount of time and energy the system has saved me has felt invaluable, even though it has meant taking out loans to pay for school. Previously, I was making up for the work the system is now doing, and when I went on this system I became aware of a renewed energy and increased capacity to focus on my schoolwork and be engaged with part of my mind that had previously been allocated solely to diabetes.
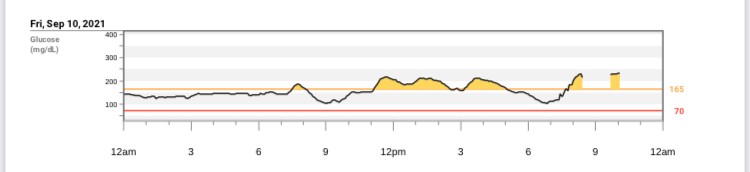
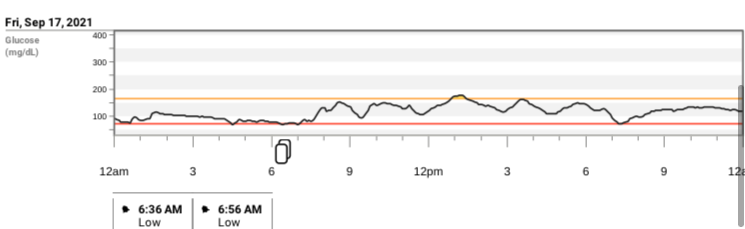
When I became sick abroad, my perception of the system as something that I had to justify to myself shifted to something that was a life-saving necessity. All the while that I was unable to eat and finding it hard to even think about diabetes, my CGM was reading my blood sugar and my insulin pump was giving me little micro-boluses to compete with its rising levels as I slowly drank soda and other fluids. By the end of the 24-48 hour period, it had given me an amount of insulin within my usual daily range, and kept me hovering from 150 – 180 mg/dl, which for me was a good sick day range. That is work I could have been doing, giving myself shots with a half-unit pen, but not nearly as precisely and definitely not as effortlessly. In fact, that would have added a new level of error that would have most assuredly brought more difficulties my way, which I say from previous sick day experiences.
It was amazing to be able to just focus on healing, instead of micro-managing blood sugar all day. In fact, once I made it through the nausea, I remember my recovery day as peaceful, rather than miserable, in part because I was not working, not in school, and not really focused on diabetes. Just resting and being cared for.
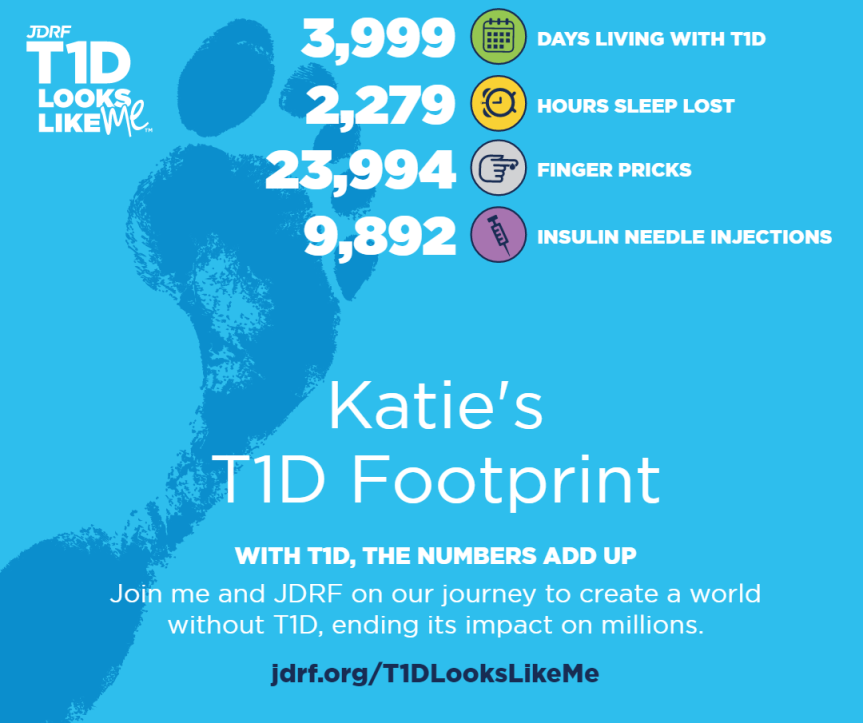
For years, in fact from the first weekend of my diagnosis, the narrative I have heard from many healthcare providers and diabetes organizations has been “if you take care of yourself, you can live a completely normal life with diabetes.” I get that this can empowering for many people, but I wondered for many years why I felt like I was failing to achieve that normalcy. Yes, I was managing to pursue my dreams, but I was working so hard, filled with anxiety, and felt like I was struggling to keep up. It might have looked normal from the outside, but from the inside, it felt like a continual marathon. Since I began using this system my life has felt a lot closer to normal – and I can barely afford it. I think my more accurate narrative for many years was, “if you work constantly, other people will think that you live a normal life, but you will know that you can keep fooling them only as long as you are willing to keep working 24/7 and say that you’re fine.” Or maybe, “you can live a normal life, but only if you have really amazing health coverage and a good deal of expendable income and supportive family and friends and adequate time off from your job…”
Now, at this point, my narrative has shifted to encompass the emotional adaptation to T1D that has been part of the journey for me. After many years of T1D I think my most accurate narrative is, “your new normal will be planning and adapting to the unexpected. It will be asking for and accepting help and meeting really amazing people who are navigating T1D too. It will be learning to rest and do less every day so that you are able to enjoy what you do. And it will be feeling like you are failing sometimes and living in fear of your health insurance coverage changing or ending.”
It makes me think that maybe if we said all of that, rather than saying, “you can live a normal life if you take care of yourself,” we would be forced to confront the need for support and the reality that without adequate, reliable, affordable access to diabetes management supplies, normalcy is a false promise. Moreover, we would take the relieve some of the burden from the person with diabetes and center it appropriately on healthcare systems, which are currently leaving many people out and bankrupting others.
I’m concerned that when I’m no longer in grad school, I will not have an insurance plan that allows me to get supplies at even the cost I currently pay, and I will have to go back to shots. It’s amazing the reservoir of mental and physical energy that going on such a system opened up for me, and I want that for anyone with T1D who is interested in such technology. That requires prioritizing insulin access as a human right. For many people in the world, shots or even vials of insulin are not guaranteed, and this is a horrific injustice. Battling supply scarcity and paying a huge chunk of your income just to have what you need to live steals the energy needed to dream and thrive. So as this amazing technology progresses, my hope is that for each advancement in diabetes tech, there is the same energy and eye to access for all people with T1D, both for the technology itself, and the insulin it requires.
*As always, I share my personal reflections on T1D and my writing is not medical advice.*










 My purpose on the ground in Bolivia became to interview, chat with, observe and learn from as many people living with Type 1 Diabetes or supporting those who do. Over the course of three weeks and five cities I got to do over 40 interviews and focus groups with nearly 100 participants made up of youth with T1D, their families, and the clinical staff and volunteers who support them. Everywhere I turned, a new element of life with diabetes in Bolivia jumped out at me. It became apparent that Bolivian cultural values were critical to consider when thinking about successful health outcomes for youth with T1D, especially the role of the family. One participant who volunteers as a leader for the group in Potosí and who has had T1D for 23 years himself, said that in all the situations he has observed, “La familia ha sido fundamental para poderlo apoyar..cree una necesidad, de, en todo diabético, de que la educación no sea sólo en el paciente diabético, pero sea también en su entorno. Ese apoyo a la familia, o esa educación a la familia, creo que también es muy importante, porque es un daño que afecta la familia” (“The family has been instrumental in that it can support…it creates a need, that, for all diabetics, the education not reach just the diabetic patient, but also their environment. This support for the family, or education for the family, I think it’s also really important, because it [diabetes} is an injury that affects the whole family”).
My purpose on the ground in Bolivia became to interview, chat with, observe and learn from as many people living with Type 1 Diabetes or supporting those who do. Over the course of three weeks and five cities I got to do over 40 interviews and focus groups with nearly 100 participants made up of youth with T1D, their families, and the clinical staff and volunteers who support them. Everywhere I turned, a new element of life with diabetes in Bolivia jumped out at me. It became apparent that Bolivian cultural values were critical to consider when thinking about successful health outcomes for youth with T1D, especially the role of the family. One participant who volunteers as a leader for the group in Potosí and who has had T1D for 23 years himself, said that in all the situations he has observed, “La familia ha sido fundamental para poderlo apoyar..cree una necesidad, de, en todo diabético, de que la educación no sea sólo en el paciente diabético, pero sea también en su entorno. Ese apoyo a la familia, o esa educación a la familia, creo que también es muy importante, porque es un daño que afecta la familia” (“The family has been instrumental in that it can support…it creates a need, that, for all diabetics, the education not reach just the diabetic patient, but also their environment. This support for the family, or education for the family, I think it’s also really important, because it [diabetes} is an injury that affects the whole family”).





